|
x |
x |
|
 |
 |
|
INFECTIOUS
DISEASE |
BACTERIOLOGY |
IMMUNOLOGY |
MYCOLOGY |
PARASITOLOGY |
VIROLOGY |
|
SLOVAK |
BACTERIOLOGY - CHAPTER
FOURTEEN
SPIROCHETES AND NEISSERIA
Dr Alvin Fox
Emeritus Professor
University of South Carolina School of Medicine
|
|
TURKISH |
|
SPANISH |
|
ALBANIAN |
|
|
Let us know what you think
FEEDBACK |
|
SEARCH |

 |
|
Logo image © Jeffrey
Nelson, Rush University, Chicago, Illinois and
The MicrobeLibrary |
|
|
|
KEY WORDS
Spirochete
Axial filament
Treponema
pallidum
Syphilis
Chancre
Primary
Lesion
Darkfield
microscopy
Secondary
Lesion
Tertiary
Lesion
Anti-cardiolipin
antibodies
Borrelia
burgdorferi
Lyme disease
Relapsing
fever
Leptospira
(leptospirosis)
Neisseria
Thayer Martin
agar
Oxidase test
N.
gonorrhoeae
Gonorrhea
N.
meningitidis
Meningitis
 Figure 1a. Annual rate of primary and secondary syphilis
cases among males and females, by race/ethnicity — National Notifiable
Diseases Surveillance System, United States, 2005–2013. CDC
Figure 1a. Annual rate of primary and secondary syphilis
cases among males and females, by race/ethnicity — National Notifiable
Diseases Surveillance System, United States, 2005–2013. CDC
 Figure 1b
Figure 1b
Umbilicus of an infant, which displayed an inflamed lesion that under a
darkfield examination revealed the presence of Treponema pallidum
spirochetes, and hence, a diagnosis of congenital syphilis. CDC
 Figure 1c
Figure 1c
The interior oral cavity of an elderly African-American male patient,
revealing a perforated hard palate due to what was a congenital syphilis
infection. At the time of this photograph, the patient was being treated
for both active syphilis, and gonorrhea infections. CDC
 Figure 2 Histopathology showing Treponema pallidum spirochetes in testis of experimentally infected rabbit. Modified Steiner silver stain.
CDC/Dr. Edwin P. Ewing, Jr. epe1@cdc.gov
Figure 2 Histopathology showing Treponema pallidum spirochetes in testis of experimentally infected rabbit. Modified Steiner silver stain.
CDC/Dr. Edwin P. Ewing, Jr. epe1@cdc.gov
|
SPIROCHETES
The most important genera of spirochetes are Treponema, Borrelia and Leptospira.
These are are Gram negative bacteria that are
long, thin, helical and motile. Axial filaments (a form of flagella) found
between the peptidoglycan layer and outer membrane and running parallel to them,
are the locomotory organelles.
Syphilis
Treponema pallidum pallidum
T. pallidum is the causative agent of syphilis, a common
sexually-transmitted disease found world-wide (figure 1a). It is generally transmitted by genital/genital contact. Transmission
in utero
or during birth can also occur (figure 1b). Syphilis, chronic and slowly progressive, is the
third most common sexually transmitted disease. After initial infection, a
primary chancre (an area of ulceration/inflammation) is seen in genital areas
(figure 4 and 6) or elsewhere (figure 3) within 10 to 60 days. The organism, meantime, has penetrated and systemically spread.
The patient has flu-like symptoms with secondary lesions particularly affecting
the skin (figure 5). These occur 2 to 10 weeks later. The final stage (if untreated) is tertiary syphilis
(several years later). In primary and secondary syphilis organisms are often
present in large numbers. However, as the disease progresses immunity controls
bacterial replication and fewer organisms are seen. It is extremely difficult to
detect spirochetes in tertiary syphilis. The systemic lesions of skin, central
nervous system and elsewhere are suggestive of a delayed hypersensitivity
reaction.
The organism cannot be cultured from clinical
specimens. Thus, experimentally, syphilis is commonly studied in animal models.
Also microscopic and serological methods are the only means of clinical
diagnosis.
In primary syphilis (before immunity develops), the
organisms are often present in sufficient numbers in exudates to be detected by
dark field microscopy. In conventional light microscopy, the light shines through
the sample and thin treponemes cannot be visualized. In dark field microscopy,
the light shines at an angle and when reflected from the organism will enter the
objective lens. The actively motile organisms appears brightly lit against the
dark backdrop. Alternatively fluorescent antibody staining is used.
In secondary and tertiary syphilis, serological
methods are usually used to detect syphilis. Screening methods are based on
detecting serum antibodies to
cardiolipin in patients (including VDRL test). The
antibodies result from tissue injury, with autoimmunity developing to self
components. Thus, there are many other diseases that result in anti-cardiolipin
antibodies and false positives are common. However, these are cheap screening
tests. More definitive diagnosis is achieved by detecting the presence of
"specific" serum antibodies against treponemal antigens. These tests
are more expensive and usually performed (as a definitive diagnosis) on sera
previously shown to be positive after first detecting antibodies to cardiolipin.
Primary and secondary syphilis occur within a year of infection and are
sometimes referred to as "early syphilis". Patients with early syphilis are
highly infectious..
Summary of Symptoms
Primary syphilis
-
Usually a single firm, round sore (but there may
be more). Usually on the genitals but can be elsewhere
-
No pain at the site of the sore
The sore will heal without intervention
Secondary syphilis
-
Rough red skin rash, often on the back (figure
6d) but can be elsewhere. The rash does not usually itch
-
Sores on mucous membranes (seen in mouth,
anus, vagina)
-
Red spots (known as syphilids) on palms of hands
and soles of feet (figure 6a, b and c)
-
Fever
-
Lymphadenopathy (swollen lymph glands)
-
Sore throat
-
Hair loss
-
Headache
-
Weight loss
-
General malaise
Symptoms will resolve with or without treatment and
the infection becomes latent.
Tertiary Syphilis
The disease, when untreated, can remain latent for
years (even two to three decades) and most infected people do not
develop further symptoms; however, if disease does reappear it can
be very serious and sometimes fatal. The symptoms include:
Epidemiology
From 2005 to 2013, the number of primary and secondary syphilis cases
reported each year in the United States nearly doubled, from 8,724 to
16,663; the annual rate increased from 2.9 to 5.3 cases per 100,000
population. Most of these cases were in men (91.1% of all primary and
secondary syphilis cases in 2013) and mostly in men who have sex with
men. The rate per 100,000 among men
increased from 5.1 in 2005 to 9.8 in 2013.
Treatment
No vaccine exists, but antibiotic therapy (usually
penicillin G) is usually highly effective, including treatment of congenital
syphilis.
Bejel
Treponema pallidum endemicum
This disease is rare (in the US) and is caused by organisms related to
T.
pallidum. T. pallidum endemicum is morphologically and serologically
indistinguishable from Treponema pallidum pallidum.
Bejel, also known as endemic syphilis, is
not transmitted sexually but via contact, for example hands to broken
skin and mouth to mouth. The disease can also be spread by sharing eating
utensils. It is a disease of low income groups with poor hygiene and
often begins in childhood.
Depending on the
route of transmission, skin or mucous membranes are the first to be
infected but the bacterium can spread deeper to the bones. Thus, one sees
sores in the mouth, throat and the nasal passages and the infected lesions
can penetrate deep into the tissue causing major malformations of the face
and limbs. This results in severe bone pain and there is also swelling of
the lymph nodes. The T. pallidum organisms can be found in swabs of
the sores.
Treatment
Treatment of bejel, which can be completely
curative, is similar to syphilis, that is penicillin G or
tetracycline.
Epidemiology
Bejel is found in the Middle-East, Africa, Australia
and central Asia. It is also known as sahel disease in West Africa.
Pinta
Treponema carateum
Pinta is another non-venereal, treponematous
disease which is caused by T. carateum. It occurs in the New World,
particularly the Caribbean, central America and northern South America.
Pinta is the Spanish for "painted". Again, it is a disease of
poor regions with sub-standard hygiene and is spread by personal contact
through cuts in the skin. This results in scaly red lesions (hence the
name) which form a lump at the site of the primary infection. Small satellite
lesions form around the primary lesion and lymph node swelling is also
seen. Some months after the primary infection, the patient experiences
more scaly red lesions that are now flat and tend to itch. These are the
pintids and occur around or distant from the site of the primary
infection. The color of the pintids changes to blue black with time
and then can lose pigmentation. Unlike bejel, the disease does not spread
deep into the tissues and bones. Detection is is via serology or direct
examination of lesion specimens under the light microscope.
Treatment
Treatment of pinta is again curative and can
be accomplished by a single injection of penicillin G.
Yaws
Treponema pertenue
Yaws (figure 7) is another chronic
treponematous disease of poor hygiene. It can be very disfiguring. It strikes
mainly children in Africa, south Asia and northern South America. The
causative agent is T. pertenue. As with pinta and bejel, spread is
via direct contact through skin lesions. About a month after the
infection, a papule forms at the infection site which transformsinto a
crusted ulcer that takes months to heal. Painful swelling of the lymph
nodes occurs. Later, soft growths appear on the face, buttocks and limbs.
They can also occur in the bottoms of the feet causing the infected person
to have a very characteristic walk which gives rise to the name of
"crab yaws". Further formation of tumors and ulcers on the face
can cause bone malformation and can be disfiguring. Microscopy (of samples
from the lymph nodes) is diagnostic and there are various serological tests.
Treatment of yaws is also a single penicillin
G injection which can be completely curative
|
 Figure 3 Primary Syphilis Bristol Biomedical Archive © University
of Bristol. Used with permission
Figure 3 Primary Syphilis Bristol Biomedical Archive © University
of Bristol. Used with permission |
 Figure 4 Primary syphilis. Primary chancre on the glans
The University of Texas Medical Branch
Figure 4 Primary syphilis. Primary chancre on the glans
The University of Texas Medical Branch
 Figure 5 Secondary syphilis - mouth mucosa Bristol Biomedical
Archive © University of Bristol. Used with permission
Figure 5 Secondary syphilis - mouth mucosa Bristol Biomedical
Archive © University of Bristol. Used with permission
 Figure 6 Primary syphilis. A vulvar chancre and condylomata acuminata
The University of Texas Medical Branch
Figure 6 Primary syphilis. A vulvar chancre and condylomata acuminata
The University of Texas Medical Branch
 Figure 6a. Secondary syphilis: Soles of both feet
of a syphilis patient revealing the presence of secondary syphilitic
lesions consisting of erosive dermal regions of the toes, mainly
involving the intertriginous spaces between the toes. CDC
Figure 6a. Secondary syphilis: Soles of both feet
of a syphilis patient revealing the presence of secondary syphilitic
lesions consisting of erosive dermal regions of the toes, mainly
involving the intertriginous spaces between the toes. CDC

 Figure 6b. Secondary syphilis: Soles of feet of a
syphilis-infected patient (plantar syphilids) in a secondary syphilitic
infection. CDC
Figure 6b. Secondary syphilis: Soles of feet of a
syphilis-infected patient (plantar syphilids) in a secondary syphilitic
infection. CDC
 Figure 6c. Secondary syphilis: Palms of hands showing palmar syphilids,
due to secondary syphilis. Rash may include forearms. CDC
Figure 6c. Secondary syphilis: Palms of hands showing palmar syphilids,
due to secondary syphilis. Rash may include forearms. CDC

 Figure 6d. Secondary syphilis: Upper back and neck of patient with a
maculopapulosquamous outbreak of nodular syphilids. CDC
Figure 6d. Secondary syphilis: Upper back and neck of patient with a
maculopapulosquamous outbreak of nodular syphilids. CDC
 Figure 7a. Yaws is a crippling and disfiguring disease affecting some 50 million people
in the world © WHO
Figure 7a. Yaws is a crippling and disfiguring disease affecting some 50 million people
in the world © WHO
 Figure 7b. Discolored areas indicative of pinta. Pathologic changes
accompanying this discoloration include thickening of the epidermis,
followed by scaliness and drying of the skin, known as acanthosis. CDC
Figure 7b. Discolored areas indicative of pinta. Pathologic changes
accompanying this discoloration include thickening of the epidermis,
followed by scaliness and drying of the skin, known as acanthosis. CDC
|
|
WEB RESOURCES
Some facts about Syphilis
CDC
Some
facts about Lyme disease
CDC |
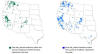
Lyme disease
Borrelia burgdorferi
Lyme disease is caused by Borrelia burgdorferi
(figure 8a,b and 13) and is a relatively newly recognized
disease. It is found widely in the United States (figure 9) but is most
concentrated in the north east and mid west. The number of cases peaked in
2009 (figure 10a).
Although clinically first described in 1975, the role of a tick-borne
spirochete was not proven until 1983. These ticks (figure 12) infect a large array of wild
life. A tick bite leads to transmission of B.
burgdorferi causing an erythematous skin rash (figure 11) in a few days along with a
transient bacteremia leading to (weeks or months later) severe neurologic
symptoms or polyarthritis. Cardiac problems may occur in a minority of cases
(figure 10c). Cases of Lyme disease occur primarily in the summer months
in the United States because of increased outdoor activities leading to
increased likelihood of picking up a tick.
If
antibiotic therapy is initiated early, a cure is usually achieved. However, late
antibiotic administration (penicillin or tetracycline) is often ineffective.
The life cycle of Lyme disease ticks is shown in figure 14a.
|
 Figure 8a Histopathology showing Borrelia burgdorferi spirochetes in Lyme disease. Dieterle silver
stain. CDC/Dr. Edwin P. Ewing, Jr.
epe1@cdc.gov
Figure 8a Histopathology showing Borrelia burgdorferi spirochetes in Lyme disease. Dieterle silver
stain. CDC/Dr. Edwin P. Ewing, Jr.
epe1@cdc.gov
 Figure 8b
Figure 8b
Under a high magnification, this digitally-colorized scanning electron
micrograph depicts three Gram-negative, anaerobic, Borrelia
burgdorferi bacteria, which had been derived from a pure culture. |
 Figure 9
Figure 9
Incidence of Lyme disease by county in the United States 2012. CDC
 Figure 10a
Figure 10a
The number of reported cases of Lyme disease from 2003 through 2012. The
number of confirmed cases ranged from a low of 19,804 in 2004 to high of
29,959 in 2009. CDC
 Figure 10b
Figure 10b
Lyme disease patients are most likely to have illness onset in June,
July, or August and less likely to have illness onset from December
through March. CDC
 Figure 10c
Figure 10c
Breakdown of reported Lyme disease cases from 2001 to 2010 by disease
manifestation. The majority of cases are the EM rash. Other
manifestations are less common, some patients have more than one
presentation. CDC
 Figure 11a
Figure 11a
Left anterior chest and shoulder region of a patient who’d presented
with the erythema migrans (EM) rash characteristic of what was diagnosed
as Lyme disease, caused by the bacterium, Borrelia burgdorferi.
CDC
 Figure 11b Lyme disease rash CDC
Figure 11b Lyme disease rash CDC
 Figure 12 Ixodes scapularis (deer tick), tick vector for Lyme disease.
Its abdomen is engorged with a host blood
meal, this image shows a lateral view of a female. CDC
Figure 12 Ixodes scapularis (deer tick), tick vector for Lyme disease.
Its abdomen is engorged with a host blood
meal, this image shows a lateral view of a female. CDC
|
 Figure 13 Morphology of Borrelia burgdorferi. Dark
field image ©
Jeffrey Nelson, Rush University, Chicago, Illinois
and The MicrobeLibrary
Figure 13 Morphology of Borrelia burgdorferi. Dark
field image ©
Jeffrey Nelson, Rush University, Chicago, Illinois
and The MicrobeLibrary
 Figure 14a Life cycle of Lyme disease ticks CDC Figure 14a Life cycle of Lyme disease ticks CDC
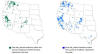 Figure 14b
Figure 14b
Tick borne relapsing fever. During the years 1990-2011, 483 cases
of TBRF were reported in the western U.S., with infections being
transmitted most frequently in California, Washington, and Colorado. CDC |
Diagnosis
B. burgdorferi is highly
fastidious, growing extremely slowly in tissue culture (not bacteriological)
media. The vast majority of body fluid or tissue samples from patients with Lyme
disease do not yield spirochetes on culture. Lyme disease is thus usually
diagnosed by detection of serum antibodies to B. burgdorferi. However,
acutely antibodies may not occur in detectable titer, making early diagnosis
difficult. However, late diagnosis may lead to ineffective
treatment. Many patients are unaware of having had a tick bite or a rash.
Etiology
The chronic arthritis clinically
resembles rheumatoid arthritis. Live agent is almost never cultivated from the
joint (in common with other forms of reactive arthritis such as Reiter's
syndrome and rheumatic fever). However, small numbers of persistent spirochetes
and borrelial antigens have been detected histologically in human tissues.
Whether the organism persists in a viable form or not remains to be determined.
Thus, there is no clear explanation for the immunopathologic stimulus for chronic
tissue injury in Lyme arthritis.
Relapsing fever
Borrelia hermsii and Borrelia
recurrentis
There are two types of relapsing fever:
- Tick-borne relapsing fever (TBRF)
- Louse-borne relapsing fever (LBRF)
Tick-borne relapsing fever occurs in the western
United States and is usually linked to sleeping
in rustic, rodent-infested cabins in mountainous
areas. Louse-borne relapsing fever is
transmitted by the human body louse and is
generally restricted to refugee settings in
developing regions of the world.
There are fewer than 100 cases of relapsing fever per year in US.
During the years 1990-2011, 483 cases of TBRF were reported in the western
United States.
Relapsing fever
(with associated bacteremia) is caused by species of Borrelia that
are transmitted by tick (Borrelia hermsii, rodent host) and lice (B.
recurrentis, human host) bites. The term relapsing fever is derived from the
following repeating cycle. As an immune response develops the disease relapses.
However, the antigens expressed change and the disease reappears.
The organism
is extremely difficult to culture and there is no serological test. The organism
is generally detected by blood smear.
|
 Figure 15 Scanning electron micrograph of Leptospira interrogans strain
RGA. Two spirochetes bound to a 0.2 µm filter. Strain RGA was isolated in 1915 by Uhlenhuth and Fromme from the blood of a soldier in Belgium.
CDC/NCID/Rob Weyant
rsw2@cdc.gov Figure 15 Scanning electron micrograph of Leptospira interrogans strain
RGA. Two spirochetes bound to a 0.2 µm filter. Strain RGA was isolated in 1915 by Uhlenhuth and Fromme from the blood of a soldier in Belgium.
CDC/NCID/Rob Weyant
rsw2@cdc.gov
 Figure 16 Leptospirosis in the kidney Bristol Biomedical
Archive © University of Bristol. Used with permission
Figure 16 Leptospirosis in the kidney Bristol Biomedical
Archive © University of Bristol. Used with permission |
Leptospirosis
There are fewer than 100 cases of
leptospirosis per year in US. This flu-like or
severe systemic disease is a zoonotic infection. Leptospira (figure
15) are transmitted
in water contaminated with infected urine from wild animals (including rodents)
and farm animals and can be taken in through broken skin (e.g. bathing). Leptospira
particularly infect the kidney (figure 16), brain and eye. They are the most readily culturable of the
pathogenic spirochetes; but this is not routine and diagnosis is usually by serology.
Treatment Leptospirosis is treated with antibiotics, such as doxycycline or
penicillin, which should be given early in the course of the disease.
Intravenous antibiotics may be required for persons with more severe
symptoms. Persons with symptoms suggestive of leptospirosis should
contact a health care provider.
|
 Figure 17a
Figure 17a
Gonorrhea — Rates by Year, United States, 1941 – 2012. CDC
 Figure 17b
Figure 17b
Gonorrhea—Rates by Age and Sex, United States, 2012. CDC
 Figure 17 c
Figure 17 c
Gonorrhea — Rates by Sex, United States, 1992 – 2012. CDC
 Figure 17d
Figure 17d
Gonorrhea — Rates by County, United States, 2012. CDC
 Figure 17e
Figure 17e
Positive FA test for Neisseria
gonorrhoeae. This strain was penicillin-resistant.
CDC
|
NEISSERIA
Neisseria
are Gram negative diplococci (pairs of cocci). These bacteria grow best on
chocolate agar (so-called because it contains heated blood, brown in color); a
modified (selective) chocolate agar commonly used is Thayer Martin. The colonies
are oxidase positive (i.e. produce cytochrome oxidase) which is demonstrated by
flooding the plate with a dye which on oxidation changes color.
N. gonorrhoeae
(the
"gonococcus")
N. gonorrhoeae
(figure
20 and 21),
found only in man, is the causative agent of gonorrhea, the second most common
venereal disease. Gonorrhea has recently declined after a peak in 1976 (figure
17a). The disease particularly occurs in younger adults (figure 17b) and is
found equally in males and females (figure 17c). Highest rates in the United
States are in the southeast (figure 17d).
N. gonorrhoeae often causes an effusion of polymorphonuclear
cells. A smear (figure 18, 19) may show the presence of Gram negative cocci present in cells.
However, culture is essential for definitive diagnosis. There is a fluorescent
antibody test (figure 17e).
A common feature of disseminated
gonoccocal disease is arthritis. Although commonly considered a form of septic
arthritis, in many cases gonococci cannot be isolated from the joint (i.e. they
are "reactive" in nature). Dermatitis is also common.
Penicillin therapy is still usually
effective. However, resistant strains producing beta lactamases are
sufficiently common that alternatives are recommended for all gonococcal
infections; this includes ceftriaxone (a beta lactamase-resistant
cephalosporin).
Because of increasing antibiotic resistance, new therapies
to treat gonorrhea have been sought. Two new antibiotic regimens using
existing drugs – injectable gentamicin in combination with oral azithromycin
and oral gemifloxacin in combination with oral azithromycin – successfully
treated gonorrhea infections in a clinical trial. The injectable gentamicin/oral
azithromycin combination appears to be 100% effective in curing genital
gonorrhea infections, and while the oral gemifloxacin/oral azithromycin
combination was 99.5% effective.
There is no vaccine since strains are highly variable in their
external antigens (both outer membrane and pili). Both are involved in the
initial adhesion of the organism to genital epithelium.
IgA proteases (also produced by N.
meningitidis) are involved in successful colonization. As for many other
bacterial infections, a role for both the lipopolysaccharide and peptidoglycan in
tissue injury have been suggested. Exotoxins are not believed to be of
importance in pathogenesis.
|
|
WEB RESOURCES
Some
facts about gonorrhea
CDC
Diagnosis
of Neisseria gonorrhoeae
CDC Division of AIDS, STD, and TB Laboratory Research |
 Figure 18 Neisseria gonorrhoeae Gram stained urethral discharge. The image shows many polymorphonuclear leukocytes (PMNs) and gram-negative extra- and intra-cellular diplococci.
Figure 18 Neisseria gonorrhoeae Gram stained urethral discharge. The image shows many polymorphonuclear leukocytes (PMNs) and gram-negative extra- and intra-cellular diplococci.
(1,000X oil) © J. Michael Miller
Centers for Disease Control and Prevention Atlanta, Georgia
and
The MicrobeLibrary
|
 Figure 19 Gram Stain from Neisseria gonorrheae Infection Urethral discharge from a male patient.
Stain shows gram-negative diplococci both intracellular and extracellular to a polymorphonuclear leukocyte or puss cell. In a symptomatic male patient, this Gram stain finding is considered diagnostic of the sexually transmitted disease caused by Neisseria gonorrheae. In female patients, one cannot use this type of finding as diagnostic of N. gonorrheae infection because the female genital tract may contain commensal Neisseria species.
© Gloria J. Delisle and Lewis Tomalty, Queens University, Kingston, Ontario
Canada and
The MicrobeLibrary
Figure 19 Gram Stain from Neisseria gonorrheae Infection Urethral discharge from a male patient.
Stain shows gram-negative diplococci both intracellular and extracellular to a polymorphonuclear leukocyte or puss cell. In a symptomatic male patient, this Gram stain finding is considered diagnostic of the sexually transmitted disease caused by Neisseria gonorrheae. In female patients, one cannot use this type of finding as diagnostic of N. gonorrheae infection because the female genital tract may contain commensal Neisseria species.
© Gloria J. Delisle and Lewis Tomalty, Queens University, Kingston, Ontario
Canada and
The MicrobeLibrary
 Figure 20 Scanning electron micrograph of Neisseria gonorrheae
© Margaret Ketterer, University of Iowa, Iowa City, Iowa
USA and
The MicrobeLibrary
Figure 20 Scanning electron micrograph of Neisseria gonorrheae
© Margaret Ketterer, University of Iowa, Iowa City, Iowa
USA and
The MicrobeLibrary
 Figure 21 Neisseria gonorrhoeae - coccoid prokaryote (dividing); causes gonorrhea
(SEM
x 40,000) ©
Dennis Kunkel Microscopy, Inc.
Used with permission
Figure 21 Neisseria gonorrhoeae - coccoid prokaryote (dividing); causes gonorrhea
(SEM
x 40,000) ©
Dennis Kunkel Microscopy, Inc.
Used with permission
|
 Figure 22
Neisseria meningitidis, group C, in spinal fluid.
CDC/Dr. M.S. Mitchell Figure 22
Neisseria meningitidis, group C, in spinal fluid.
CDC/Dr. M.S. Mitchell
 Figure 23 Neisseria meningitidis - coccoid prokaryote (dividing); causes meningitis and
Waterhouse-Friderichson syndrome (a fulminating meningococcal infection occurring mainly in children under ten years old) ©
Dennis Kunkel Microscopy, Inc.
Used with permission
Figure 23 Neisseria meningitidis - coccoid prokaryote (dividing); causes meningitis and
Waterhouse-Friderichson syndrome (a fulminating meningococcal infection occurring mainly in children under ten years old) ©
Dennis Kunkel Microscopy, Inc.
Used with permission
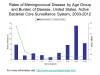
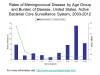 Figure 24
Figure 24
Rates of meningococcal disease in the United States by age group. CDC |
Neisseria meningitidis (the "meningococcus")
This organism (figure 22 and 23) resides only in man. The
majority of cases are sporadic cases most commonly seen among young children
(figure 24).
Outbreaks occur usually among adults living in confined and crowded conditions
(e.g. university dorms, army barracks, prisons). Initial infection of the upper respiratory tract
(involving binding by pili) leads to invasion into the bloodstream and from
there to the brain. Indeed, it is the second most common cause of meningitis (pneumococcus
is the most common). Neisseria meningitis is usually fatal if untreated but responds well to antibiotic
therapy. Thus, rapid diagnosis is important. The organism is often detectable in
spinal fluid (Gram negative diplococci within polymorphonuclear cells) or
antigenically. Culture on Thayer Martin (or similar) agar is essential for
definitive diagnosis. Penicillin is the drug of choice.
Meningococci vary antigenically and
can be serogrouped with anti-capsular antibodies. The capsule is an important
pathogenesis factor allowing inhibition of phagocytosis.
There are effective meningococcal vaccines that protect
against most types of meningococcal disease, although they do not
prevent all cases. There are two vaccines against Neisseria
meningitidis available in the United States: meningococcal
polysaccharide vaccine (Menomune) and meningococcal conjugate vaccine (Menactra,
Menveo and MenHibrix). In the United States, vaccines are approved and
routinely used against serogroups C and Y (in addition to A and W, which
circulate globally), but not B. A serogroup B meningococcal vaccine that
is licensed for use in Europe, Canada, and Australia has been used in
the United States to help control 2 outbreaks of this disease in
universities.
Non-pathogenic species morphologically
resembling Neisseria are found in the normal flora of the oropharynx but
can be differentiated from the pathogenic Neisseria readily. These
occasionally cause opportunistic human disease (including pneumonia).
|
|
|
 Return to the Bacteriology Section
of Microbiology and Immunology On-line Return to the Bacteriology Section
of Microbiology and Immunology On-line
This page last changed on
Friday, March 04, 2016
Page maintained by
Richard Hunt
|
 Figure 3 Primary Syphilis Bristol Biomedical Archive © University
of Bristol. Used with permission
Figure 3 Primary Syphilis Bristol Biomedical Archive © University
of Bristol. Used with permission Figure 8a Histopathology showing Borrelia burgdorferi spirochetes in Lyme disease. Dieterle silver
stain. CDC/Dr. Edwin P. Ewing, Jr.
epe1@cdc.gov
Figure 8a Histopathology showing Borrelia burgdorferi spirochetes in Lyme disease. Dieterle silver
stain. CDC/Dr. Edwin P. Ewing, Jr.
epe1@cdc.gov  Figure 13 Morphology of Borrelia burgdorferi. Dark
field image ©
Jeffrey Nelson, Rush University, Chicago, Illinois
and The MicrobeLibrary
Figure 13 Morphology of Borrelia burgdorferi. Dark
field image ©
Jeffrey Nelson, Rush University, Chicago, Illinois
and The MicrobeLibrary Figure 15 Scanning electron micrograph of Leptospira interrogans strain
RGA. Two spirochetes bound to a 0.2 µm filter. Strain RGA was isolated in 1915 by Uhlenhuth and Fromme from the blood of a soldier in Belgium.
CDC/NCID/Rob Weyant
rsw2@cdc.gov
Figure 15 Scanning electron micrograph of Leptospira interrogans strain
RGA. Two spirochetes bound to a 0.2 µm filter. Strain RGA was isolated in 1915 by Uhlenhuth and Fromme from the blood of a soldier in Belgium.
CDC/NCID/Rob Weyant
rsw2@cdc.gov
 Figure 17a
Figure 17a Figure 18 Neisseria gonorrhoeae Gram stained urethral discharge. The image shows many polymorphonuclear leukocytes (PMNs) and gram-negative extra- and intra-cellular diplococci.
Figure 18 Neisseria gonorrhoeae Gram stained urethral discharge. The image shows many polymorphonuclear leukocytes (PMNs) and gram-negative extra- and intra-cellular diplococci.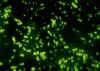 Figure 22
Neisseria meningitidis, group C, in spinal fluid.
CDC/Dr. M.S. Mitchell
Figure 22
Neisseria meningitidis, group C, in spinal fluid.
CDC/Dr. M.S. Mitchell